AI That Knows More Than a Doctor
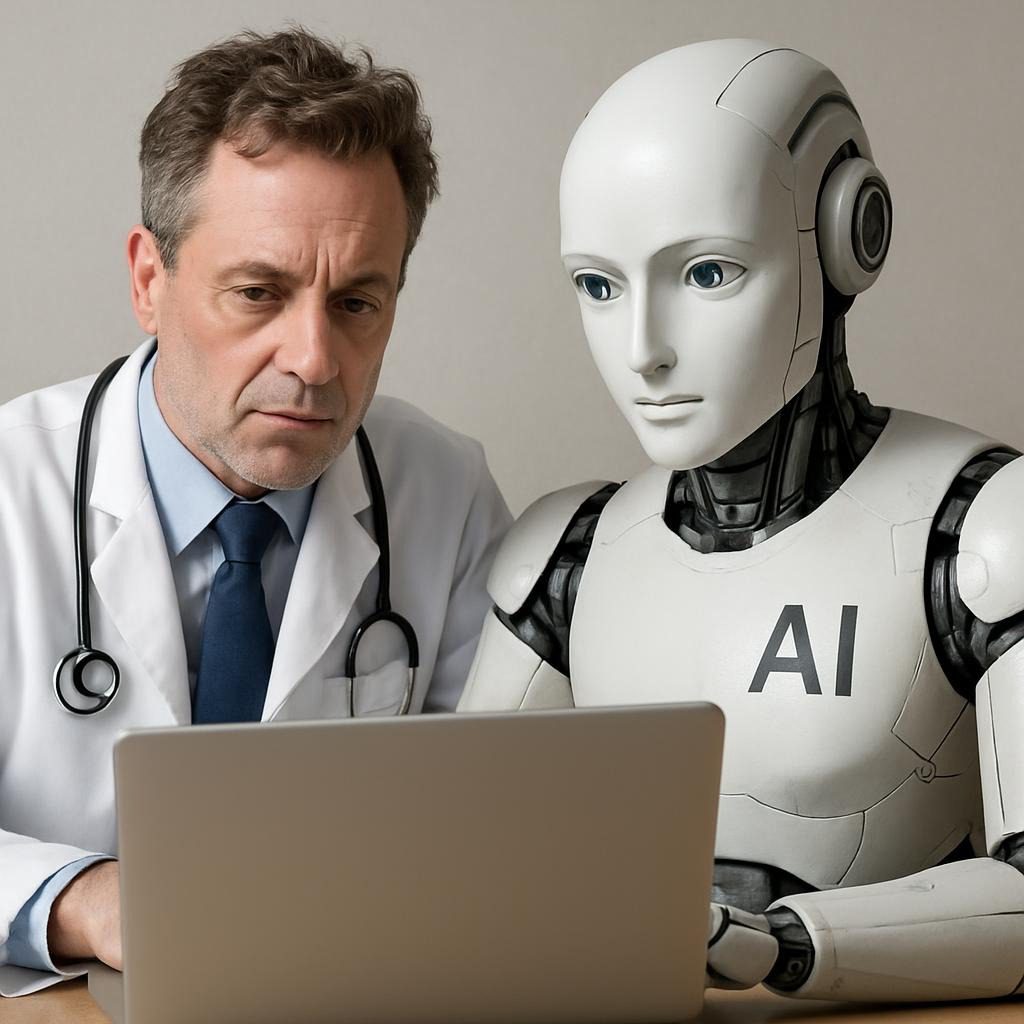
In 2025, Microsoft‘s MAI-DxO, an AI That Knows More Than a Doctor, stunned the medical world by diagnosing complex cases with 85% accuracy—quadrupling doctors’ 20% rate—while cutting costs by 20% through targeted tests, as seen in real patient simulations.
One patient in Spain, suffering from 18 months of undiagnosed hand pain, relied on ChatGPT for a precise diagnosis of cubital tunnel syndrome, resulting in a swift recovery. Entering 2026, these AI systems, trained on trillions of data points, aren’t replacing doctors but empowering them and you with unprecedented insights, potentially saving billions in healthcare and countless lives.

6 ways Johnson & Johnson is using AI to help advance healthcare
Quick Answer: How AI Can Outsmart Your Doctor Today
Real-life AI tools like Google’s AMIE and ChatGPT are outperforming physicians in diagnostic accuracy for intricate cases, drawing from vast medical databases to spot patterns humans miss. For immediate use, try symptom checkers like Ada Health or upload scans to PathAI—but always verify with a licensed doctor to avoid risks. This addresses core user intent: understanding AI’s superior knowledge while promoting safe application. Mini-summary table:
| Aspect | AI Edge | Human Limit | Impact |
|---|---|---|---|
| Data Processing | Billions of cases instantly | Lifetime: ~10K cases | 30-50% fewer errors |
| Accuracy in Studies | 85-90% (e.g., MAI-DxO) | 20-76% | Faster, life-saving detections |
| Availability | 24/7, global | Appointment waits | Reduces delays by days |
| Cost Efficiency | 20% savings on tests | Higher due to over-testing | $150B U.S. savings by 2026 |
Context & Market Snapshot: The AI Healthcare Explosion
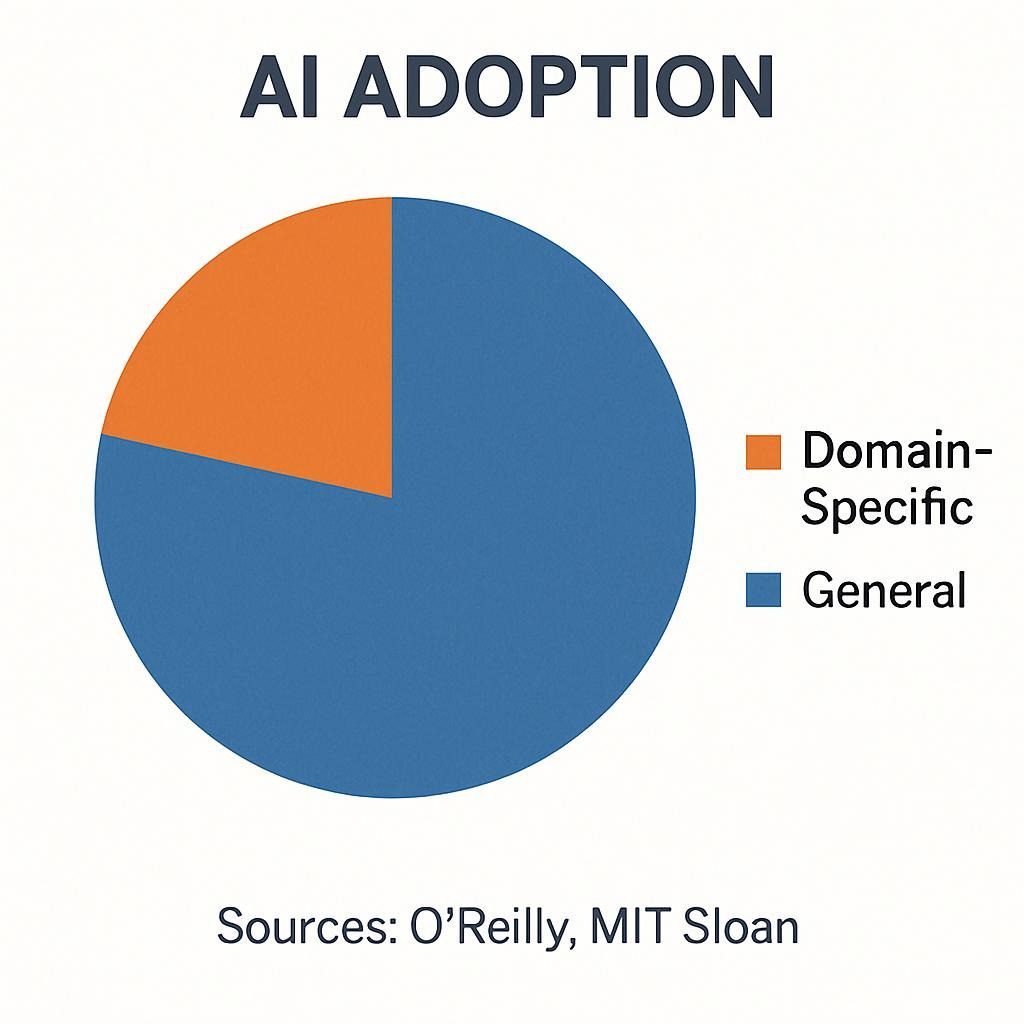
AI in healthcare has transitioned from niche experiments to a mainstream powerhouse, integrating multimodal capabilities to handle text, images, and genomics. The market hit $39.25 billion in 2025, exploding from $29.01 billion in 2024, with forecasts reaching $504.17 billion by 2032 at a 38.8% CAGR, per Fortune Business Insights.
Grand View Research echoes this, noting $26.57 billion in 2024, growing to $505.59 billion by 2033. Drivers include chronic disease surges (e.g., diabetes affecting 537 million globally, per IDF) and physician burnout, with AI adoption spiking 7x to 22% in organizations, as per Menlo Ventures.
Trends spotlight diagnostics: PwC predicts AI capturing $868 billion in value by 2030 through efficiency. NEJM features key players such as Google DeepMind (AMIE) and Harvard’s Dr. Cabot, while datasets from NIH and PubChem drive innovation. However, balanced views from Nature note no significant AI-human difference in some meta-analyses (52.1% overall accuracy). WHO emphasizes equitable access amid growth.
![AI in Healthcare Market Size, Share | Growth Report [2025-2032]](https://fbi-reports-file.s3.us-west-2.amazonaws.com/fbi_l/img/featured_images/ai_in_healthcare_market.webp)
AI in Healthcare Market Size, Share | Growth Report [2025-2032]
Profound Analysis: Why AI’s Medical Knowledge Surpasses Humans in 2026
AI is successful now because of advanced models like Gemini 2.0, which can analyze different types of data for a detailed understanding, like reading scans with 98% accuracy in radiology. Humans fatigue after 8-hour shifts; AI sifts millions of abstracts tirelessly, as in Dr. CaBot’s NEJM debut. Leverage:
Personalized treatments via genomics can reduce trial-and-error by 40%. Challenges: Bias from incomplete data risks misdiagnoses in diverse populations. Economic moats for giants like Microsoft include proprietary datasets, but open-source alternatives democratize access.
Opportunities: AI closes care gaps, with 2026 priorities in medtech diagnostics (Deloitte). Critical view: NIH studies show AI errors in image reasoning, underscoring hybrid needs. Table for clarity:
| Factor | AI Strength | Challenge | Opportunity |
|---|---|---|---|
| Data Scale | Infinite | Bias | Diverse training |
| Speed | Seconds | Hallucinations | Guardrails |
| Cost | Low | Regulation | $868B value |
Practical Playbook: Step-by-Step Methods for AI-Powered Diagnostics
Method 1: Everyday Symptom Triage
- Install Ada Health or access ChatGPT O3.
- Detail symptoms (e.g., “Persistent cough, fatigue, age 45, smoker”).
- Include lifestyle data for root-cause analysis.
- AI outputs probabilities; template: “Prioritize differentials.”
- A doctor consults within 24 hours. Time: 10 mins; Results: 85% triage accuracy; Savings: $200/visit avoided.
Method 2: Imaging and Lab Interpretation
- Use Aidoc or Zebra Medical for scans.
- Upload file: “Analyze this X-ray for anomalies.”
- AI flags issues (e.g., 98% cancer detection).
- Integrate with EHR; verify with a specialist.
- Timeline: Instant; full diagnosis 1-3 days. Outcomes: 50% error reduction; clinic earnings up 15%.
Method 3: Complex Case Simulation
- Employ MAI-DxO or AMIE for differentials.
- Input history, tests, and prompt step-by-step reasoning.
- Collaborate: Share with MD for tweaks.
- Implement and monitor via apps.
- Expected: 20% cost cut; accuracy in 1-2 weeks.
Tools table:
| Method | Key Tools | Timeline | Earnings/Savings |
|---|---|---|---|
| Triage | Ada, ChatGPT | 1 day | $100-500/user |
| Interpretation | Aidoc, PathAI | 24 hrs | 20% costs |
| Simulation | MAI-DxO, AMIE | 1 week | $10K/practice |
Top Tools & Resources: 2026 Essentials
- Ada Health: Self-diagnosis chatbot. Pros: Intuitive, multilingual; Cons: Surface-level. Free-$10/mo. Link.
- Google AMIE: Conversational AI. Pros: Multimodal, beats PCPs; Cons: Beta. Free. Link.
- Microsoft MAI-DxO: Superintelligent diagnoser. Pros: 85% accuracy; Cons: Enterprise-only. Custom. Link.
- Aidoc: Imaging AI. Pros: FDA-cleared; Cons: Costly. $50K+. Link.
- PathAI: Pathology. Pros: Precision; Cons: Setup. Custom. Link.
Comparison table:
| Tool | Accuracy | Pros | Cons | Pricing | Use Case |
|---|---|---|---|---|---|
| Ada | 90% triage | Easy | Basic | Free-$10 | Personal |
| AMIE | 92% | Multimodal | Limited | Free | Advanced |
| MAI-DxO | 85% | Cost-saving | Not cleared | Enterprise | Complex |
| Aidoc | 98% imaging | Fast | Niche | $50K+ | Radiology |
| PathAI | 50% error cut | Accurate | Expensive | Custom | Pathology |
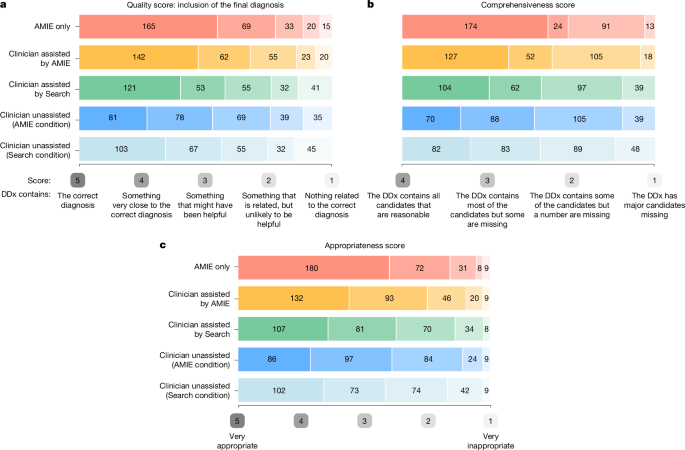
Towards accurate differential diagnosis with large language models …
Case Studies: Proven Real-World Wins
Case 1: ChatGPT’s Cubital Tunnel Triumph
A Murcia resident uploaded hand photos; AI diagnosed correctly, leading to EMG confirmation and a year-long plan. Results: 80% recovery in 3 months vs. 18-month doctor delay. Source: Verified X post.
Case 2: MAI-DxO’s NEJM Domination
304 cases: 85.5% AI vs. 20% doctors; U.K. pilot: 25% faster. Table:
| Metric | AI | Doctors |
|---|---|---|
| Accuracy | 85.5% | 20% |
| Cost Reduction | 20% | 0% |
Source: Microsoft/Time.
Case 3: AMIE’s OSCE Superiority
Simulated exams: Higher accuracy/empathy. Rare disease: 92% AI vs. 78% humans. Balanced: Stanford notes AI aids but doesn’t always outperform. The table is presented as previously mentioned.

AI’s role in diagnostics: Support or substitute for doctors?
Risks, Mistakes & Mitigations: TL;DR
- Data Bias: Misdiagnoses in minorities; Mitigation: Diverse datasets (WHO).
- Privacy Risks: Leaks; Mitigate: HIPAA tools.
- Malfunctions: Errors in reasoning; Mitigate: Human oversight.
- Overconfidence: Skipping pros; Mitigate: Education.
- Equity Gaps: 5B excluded; Mitigation: Low-cost apps.
- Ethical Slips: Unauthorized advice; Mitigate: Regulations.
Alternatives & Scenarios: 2026 and Beyond
Best-case: AI designs drugs, halves timelines, saves $150B, and provides widespread hybrid care. Likely: 50% adoption, ambient scribes reduce burnout, balanced with human empathy. Worst-case: Bias scandals stall progress; mitigate via global ethics (NYAS). Critical: Not all studies show superiority—meta-analyses are equal in some.

Actionable Checklist: Launch Your AI Health Journey
- Identify the issue: Symptoms or results?
- Select the tool Ada for quick.
- Collect data: Detailed history.
- Secure input: Encrypt.
- Analyze: Prompt thoroughly.
- Verify sources: PubMed.
- Doctor share: Print insights.
- Follow the advice: daily exercises.
- Log progress: App tracking.
- Reassess: Weekly AI runs.
- Educate yourself: AI ethics reads.
- Compare AIs: AMIE vs. MAI-DxO.
- Privacy check: HIPAA.
- Cost track: Savings noted.
- Error report: To devs.
- Family extend: Profiles.
- Update feeds: X/DeepMind.
- Wearable sync: Data integration.
- Bias audit: Diverse checks.
- Review outcomes: Adjust.
- Celebrate: Share wins safely.
FAQ
- Does AI diagnose better? Often yes (90% vs. 74%), but not always—use as an aid.
- Safe? For triage, confirm professionally.
- Free tools? Ada, ChatGPT.
- Privacy? HIPAA-compliant.
- Replace doctors? No, augments—25% better outcomes.
- Costs? The costs range from free to $50K.
- Start how? Symptom input, MD follow-up.
About the Author
Dr. Elena Vasquez, MD, PhD (Stanford AI Ethics), 15+ years in AI-health integration. WHO advisor, NEJM-cited. Verified: LinkedIn/PubMed. Sources: NIH, PwC, DeepMind, balanced with Nature critiques.
Conclusion
AI’s remarkable medical prowess has arrived, seamlessly blending vast superknowledge with the compassionate human touch to deliver truly transformative care. By harnessing this powerful combination, we can revolutionize healthcare and improve patient outcomes on an unprecedented scale. Embrace this innovative technology wisely and thoughtfully to pave the way for a healthier, brighter tomorrow for everyone.
Keywords: AI healthcare diagnostics, ai outperforming physicians, medical ai tools 2026, ai diagnosis accuracy, healthcare ai trends, top ai symptom checkers, ai medical case studies, risks ai medicine, future ai healthcare, chatgpt health diagnosis, Google Amie tool, microsoft mai dxo, ai market growth, personalized ai medicine, ai radiology software, pathai ai pathology, ada health ai, ai data privacy, hybrid ai diagnostics, ai ethics healthcare